Understanding Intensive Care Staffing, Occupancy and Capacity
For every occupied intensive care bed, there is a patient. A loved one.
Bed occupancy (used beds) and capacity (total beds) numbers are important to understand demand and pressure, but to our multi-professional teams, each and every person is important. We will always do our best to give compassionate care to the highest standard.
Our intensive care teams are working hard to provide the best levels of care for every patient. We ask that those reporting intensive care data ensure it is explained accurately and clearly so that it reflects the reality of what is happening in our intensive care units.
We need the right number and skill mix of intensive care workers to care for patients in our beds. An ICU bed without staff is like having the shell of car (the ICU bed) with an engine (the monitors and equipment), fuelled and ready to go, but has no driver (the trained, skilled staff).
We will focus on some key definitions to help ensure data is presented accurately.
- Baseline ICU bed capacity is the funded and fully staffed number of ICU beds in a hospital. Baseline occupancy is how many of these beds are full.
- Surge ICU bed capacity is the baseline ICU bed capacity plus any additional ICU beds created, for example when there is an expansion because of an emergency situation such as the current pandemic. Surge occupancy is how many of these beds are full.
- % ICU bed occupancy relative to baseline is the overall (baseline and additional) number of beds occupied relative to the baseline capacity.
Example:
Hospital X has a 20-bed ICU. The ICU is fully staffed for these beds. This means that the baseline ICU bed capacity is 20 beds. The ICU is full - all 20 beds are occupied. This means that the baseline ICU bed occupancy is 100% (20/20). There are increasing number of critically ill patients with COVID being admitted to the hospital X. The hospital decides to create an extra 20 ICU beds in another part of the hospital. This means that the surge ICU bed capacity is 40 beds (20+20). There are no additional trained ICU staff. More patients with COVID are admitted and 10 of the extra 20 ICU beds are filled. The other 20 beds remain full, so the surge bed occupancy is now 30 patients (20+10) in ICU in the hospital. The % ICU bed occupancy relative to baseline is 150% (30/20).
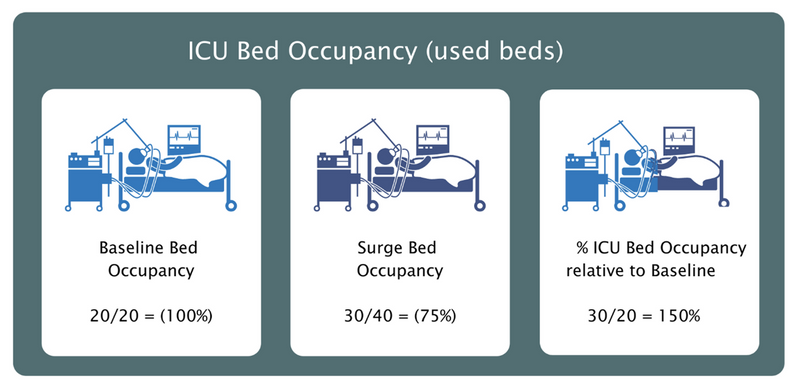
Data which only reports % surge ICU bed occupancy and without it being clear it is not % ICU bed occupancy relative to baseline is unhelpful. In the example used, hospital A could have a reported ‘75% bed occupancy’ (30 occupied beds of a total of 40 surge capacity beds). The surge bed occupancy is 75% and the % ICU bed occupancy relative to baseline is 150%
We request that reporting of ICU data MUST include the % ICU bed occupancy relative to baseline and encourage numbers and percentages to be published.
The consequences of using Intensive care surge beds includes:
- Dilution of intensive care trained staff-to-patient ratios
- Redeployment of staff from other areas. This typically includes anaesthetic and theatre staff as well as other acute specialties
- Use of areas within the hospital that are intended for other specialty care. This typically includes other high care areas as well as theatre recovery and sometimes operating rooms.
- Reduced ability to sustain all planned and urgent surgery because of the requirement to use theatre staff and space.
- Significant risk of fatigue and burnout of staff because of a need to work longer, more frequently and spreading themselves more thinly whilst caring for people with serious life-threatening conditions.
The provision of Intensive care surge beds is not part of normal practice nor is the use of additional redeployed non-intensive care staff or diluting staff-to-patient ratios. This is far from ideal and is outside the national standards during non-pandemic situations (GPICS version 2) This is however an unprecedented situation requiring new staffing guidance to try to keep patients safe (NHSE staffing guidance).
This is being achieved by support from other services, mutual aid and personal sacrifice to the workforce both physically and mentally. We ask everyone to keep following the Government guidelines and continues to maintain the fundamentals of #HandsFaceSpace.
We cannot emphasise enough that healthcare services are very much open for business and if you are feeling unwell and in need of medical help, please do not hesitate to access these services - You will be cared for.
In order to understand the strain on Intensive Care services we ask that published national and media reports include the following information when describing the number of beds occupied:
- Baseline ICU Bed Capacity is the number of funded and fully staffed intensive care beds.
- Baseline ICU Bed Occupancy is the number or % of funded and fully staffed intensive care beds which are full.
- Surge ICU Bed Capacity is the number of funded intensive care beds the extra intensive care surge beds.
- Surge ICU Bed Occupancy is the number or % of intensive care surge beds which are full.
- ICU bed occupancy relative to baseline is the number of overall (baseline and additional) beds occupied relative to the baseline capacity.
In addition, we need to report how much clinical activity has been stopped to enable the surge beds to be staffed. Reporting pandemic CRITCON-PANDEMIC levels, the number of elective and urgent surgery cases cancelled will provide a more detailed and accurate understanding of the pressure on intensive care and hospital services.
Every hospital submits their daily operational performance reports nationally to create a national situation report (sitrep) and Directory of Services (DoS) which then indicates the pressures on each hospital and region. This data must be accurate and responsibly reported.
Additional information and references:
The intensive Care Society with the Faculty of Intensive Care Medicine and NHSE have produced robust guidance on the standards expected of any intensive care area, including surge capacity. More details can be found here:
- Guidelines for the Provision of Intensive Care Services. Edition 2. Published by the Intensive Care Society and the Faculty of Intensive Care Medicine. June 2019
- Emergency Staffing for COVID-19
- ICS statement as part of the UK Critical Care Nursing Alliance (UKCCNA). The Alliance consists of nursing representatives from The Intensive Care Society, Royal College of Nursing (RCN), British Association of Critical Care Nurses (BACCN), Critical CareNational Network Nurse (CC3N), National Outreach Forum, Paediatric Critical Care Society (PCCs)
- The NHS has always demonstrated an ability to provide a short-term response to increased demand and this is now needed more than ever. Where intensive care capacity is not adequate to meet local demands, the following will be required:
- Staff: The numbers of nurses, doctors, practitioners and allied health professionals with the knowledge and technical skills to look after the sickest patients in hospital will need to be increased. There is a not a surplus of staff and it takes many years to train each of them to acquire the knowledge and technical skills needed to treat critically unwell patients. This means that provision of suitably trained staff requires existing ones to work longer hours and more shifts and/or re-deploy staff who have some of the essential skills from other areas (typically theatres, anaesthetics and other acute specialties) to support.
- Space: Expanding the intensive care footprint requires reconfiguration of other areas to accommodate surge beds. These beds require the use of designated areas within hospitals which have certain mandated specification (including oxygen provision and piping) and a range of equipment, which include ventilators and other essential devices. The reconfiguration of hospital beds to increase intensive care surge beds means that other hospital beds will be reduced with resulting pressure on other services.
- Support: Decompressing ICUs require careful consideration of mutual aid transfers to other hospitals that have available ICU capacity, as well as a reduction in elective and then urgent surgery, to release staff and space



